Cancer
Diabetes is a condition where the amount of glucose (sugar) in your blood is too high. Insulin helps the glucose move from the blood to our cells, and in diabetics the insulin is not working correctly. All carbohydrates that we eat affect our blood glucose including both starchy carbs (like bread, rice, pasta and potatoes), and sugary carbs (like sweets, chocolate, biscuits, jams, fruit and milk).
The most common types of Diabetics are Type 1, Type 2 and Gestational Diabetes.
Type 1 Diabetes is an autoimmune condition where the body's own immune system attacks the cells in the pancreas which produce insulin. This results in blood glucose levels being too high because the pancreas cannot produce insulin.
People with Type 1 Diabetes need to monitor their glucose levels so they can keep their blood glucose levels within the target range. They need to know what to do when their blood glucose is too high, or too low, and which diet and lifestyle factors could cause their glucose levels to change.
When diagnosed with Type 1 Diabetes, a Diabetes Specialist Dietitian can offer you support and education to learn more about diabetes, carbohydrate counting and insulin management.
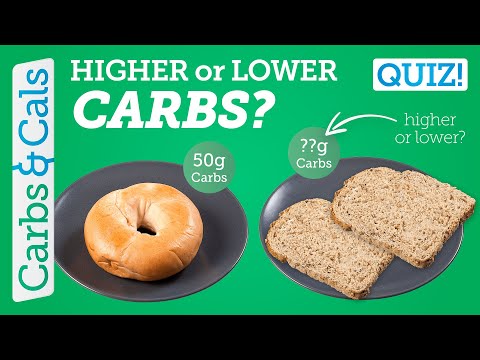
People with Type 1 Diabetes should follow a normal healthy diet, including the food groups from the Eatwell Guide. Carbohydrates have the biggest impact on blood glucose. Patients should learn about carbohydrate counting, and adjusting their insulin dose dependent on the amount of carbohydrates eaten. Low carbohydrate diets are not recommended for people with Type 1 Diabetes.
Exercise and physical activity can impact your blood glucose, but it is important to include regular physical activity as part of a healthy lifestyle. Dietitians and other health professionals can help you learn about balancing blood glucose levels whilst exercising.
Here at CDDFT, we support patients with access to an educational course to support Type 1 Diabetics - DAFNE. DAFNE 'Dose Adjustment for Normal Eating' is for Type 1 Diabetics on A Basal Bolus Insulin Regime. The course tends to be delivered face-to-face in small groups, or can be accessed remotely though MS Teams.
Type 2 Diabetes is a condition where the pancreas doesn't produce enough insulin, or where the insulin that is produced does not work correctly (insulin resistance). This results in blood glucose levels being too high because there is not enough insulin to break down the glucose.
Some people with Type 2 Diabetes will need to monitor their glucose levels so they can keep their blood glucose levels within the target range, and some may be treated with insulin and other medications.
When diagnosed with Type 2 Diabetes, a Diabetes Specialist Dietitian can offer you support and education to learn more about diabetes, including offering support around healthier diet and lifestyle changes.
People with Type 2 Diabetes are encouraged to make diet and lifestyle changes to manage the risks of complications. This could include losing weight if they have obesity or overweight, following a diet lower in carbohydrates, higher in fibre, or by counting carbohydrates. It may be suggested that following a Mediterranean-style diet could help including; lower salt, sugar and processed foods, more wholegrains, vegetables, fish and nuts.
Carbohydrates have the biggest impact on blood glucose, so many patients find it useful to reduce the amount of carbohydrates to help control their blood glucose levels.
Regular exercise and physical activity are an important part of a healthy lifestyle. Being active can help control blood glucose and keep the insulin working effectively. It can also help with losing weight, supporting mental wellbeing and reduce risk of other complications. Aim for at least 150 minutes every week, spread throughout the week.
Locally, patients with Type 2 Diabetes can access an educational platform, Desmond, provided by North Tees and Hartlepool NHS Foundation Trust
Gestational Diabetes is a condition that occurs during pregnancy, where the pancreas doesn't produce enough insulin to meet the extra needs during pregnancy. It can happen at any stage of pregnancy but is more common in the second or third trimester and most people return to normal after the baby is born.
To manage blood glucose during pregnancy, people with gestational diabetes will be encouraged to monitor their blood sugar, and make dietary changes to keep their blood sugar within the target range. Some people may also be given medication e.g. insulin.
A dietitian can give you advice on eating a healthy diet. This could include eating regularly and avoiding skipping meals, choosing higher fibre carbohydrates, eating plenty fruit and vegetables and avoiding sugary foods and drinks.
If the Gestational Diabetes is not well managed, there can be problems with the pregnancy such as the baby growing larger than usual, too much amniotic fluid in the womb, pre-mature birth, high blood pressure and more, therefore regular scans may be offered to monitor the baby. Having gestational diabetes also increases the risks of developing Type 2 Diabetes in the future.